This is the second hypothetical case discussion based on real cases submitted to the Resuscitology Team for analysis and debrief on the Resuscitology Course. Course participants are asked: “Please describe a resuscitation case that you have been involved in or witnessed that you feel (a) either had great learning points for other people on the course or (b) you feel didn’t go as well as it should and would appreciate the chance to analyse and discuss it.”
Case details are removed or altered to guarantee anonymity and confidentiality while preserving learning points. Cases are shared with the permission of the submitting clinician.
This case discussion was facilitated and summarised by Cliff Reid
60 year old male with End Stage Renal Disease (ESRD). Admitted to ICU after a MET call for possible sepsis.A formal echo showed severe LV systolic dysfunction, severe aortic stenosis, and RV dysfunction.
Three hours into the ICU admission he became peri-arrest. He was grey in colour, distressed and c/o central chest pain or pressure. He became hypotensive and was peri-arrest for about one hour, then arrested.
The patient’s young family was outside watching and crying. We had a lot of staff in the room and outside helping. Possibly too many, but it was useful to have a good line up for CPR. An airway was established early on in the code. And the person on the airway was watching the art line and ETCO2 for effective CPR and providing some coaching. It was chaotic, but we had good role allocation.
The cardiac arrest resuscitation lasted 30 minutes before being discontinued. He was mostly in a non-shockable rhythm.
There was a comment made afterwards, a concern by the person doing airway that he may have been aware/semi-conscious during part of the arrest.
Resuscitology Discussion Points
1. Cardiac arrest in ESRD patients.
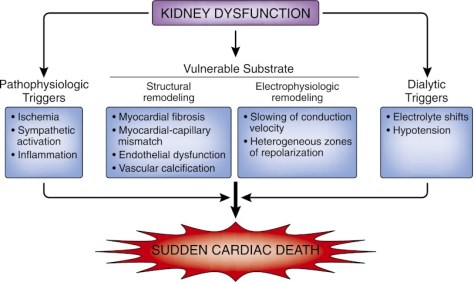
The prognosis from cardiac arrests is even worse in patients with kidney dysfunction in which survival probability decreases with a declining GFR. Among patients with ESRD who have a witnessed cardiac arrest at an outpatient dialysis facility, more than three-quarters are not discharged alive from the hospital. Structural and electrophysiologic remodeling of the heart, vascular calcification and fibrosis, autonomic dysregulation, and volume and electrolyte shifts are some of the underlying processes thought to explain the increased predisposition for sudden cardiac death in people with chronic kidney disease.(1)
2. Establishing goals of care
This patient has significant co-morbidity and severe physiological derangement and is therefore likely to have a grim prognosis. It is key to establish the patient’s wishes and minimise unnecessary suffering or futile interventions. On the other hand, curable causes of deterioration such as sepsis or pulmonary embolism may be present and early aggressive resuscitation and investigation are likely to be appropriate for this chronologically relatively young patient.
Often a parallel approach is required: aggressive resuscitation at the bedside and a concurrent discussion about the patient’s wishes with the relatives. A useful question to pose to relatives, used by Chris Nickson (often more appropriate further along into an ICU stay) is: “If he could talk to us now, what would he say about this?”
3. Likely causes of his arrest and their prevention / management
The underlying causes of haemodynamic deterioration can be rapidly differentiated into problems of relative or absolute hypovolaemia, pump dysfunction, or obstructive causes (pulmonary embolism, tamponade, tension pneumothorax)(2). Clinical assessment combined with point of care ultrasound (POCUS) allows immediate selection of fluids, vasopressors, inotropes, cardiac management, or surgical or decompressive procedures. An early blood gas can identify haemodynamically significant electrolyte derangement, in particular ionised hypocalcaemia.

In this patient’s case the presence of both severe aortic stenosis and right ventricular dysfunction contribute to significant haemodynamic management challenges. He may require emergent procedural intervention such as balloon aortic valvuloplasty and senior intensive care, cardiothoracic, and cardiology personnel would need to be mobilised. In a non-tertiary centre or middle-of-the-night scenario this could bring its own challenges and frustrations.
4. Team and communication factors
Following admission to ICU, he was peri-arrest for around one hour prior to arresting. The management of a crashing hypotensive patient like this requires a team approach and an appropriate degree of resuscitative momentum. It is critical that senior doctors and nurses are mobilised to the bedside and that the mental model is shared that immediate resuscitation is required. If this is not happening then appropriately assertive but non-judgmental / non-confrontational language should be used by the nursing or junior medical staff to highlight the urgency of the case. Examples are:
- “I am very concerned about this patient who is deteriorating”
- “I need your help immediately with the assessment of this severely shocked patient”
- “Do you want me to start adrenaline or noradrenaline while you echo him to work out what’s going on?”
- “I’ll call the registrar/fellow/consultant as it looks like we’re going to need lots of pairs of hands”
5. Management of the cardiac arrest on the ICU
The presence of invasive arterial monitoring allows chest compressions to be optimised in terms of location, rate and depth to titrate to an optimal diastolic blood pressure to support coronary perfusion. It allows early identification of ROSC and also titration of vasopressor doses to a target blood pressure rather than blindly administering 1mg doses of adrenaline (3). Continuous waveform capnography allows identification of tracheal tube placement and, like arterial blood pressure monitoring, can assist in optimisation of chest compressions, and identification of ROSC.

Crowd control is important. As additional team members arrive at different times but all wanting information regarding the case and their role, it can be helpful to allocate a ‘meet and greet’ person to update them and to protect the team leader from distraction. This ‘Resus Marshal’ can also police the number of people at the bedside and ensure non-contributors remain ‘behind the line’.
6. The ‘awake’ CPR patient
If CPR is sufficiently effective to perfuse the brain (its goal) then awareness and even full consciousness is possible. This has certainly been witnessed many times with mechanical CPR devices. While it is likely that staff may be more likely to remember this than the patient, the inevitable discomfort and distress can be mitigated with sedatives and analgesics. Ketamine provides both and would be the recommendation of most of the Resuscitology faculty. Fentanyl and/or midazolam may be considered as alternatives or in addition to ketamine. Some services have developed protocols for this situation(4).
7. Learning as a team from suboptimal cases
A full debrief is ideal but often hard to achieve. A ‘hot debrief’, conducted briefly by the team immediately after the event, can identify learning points and also review what worked well, leading to action points to take forward. Once such method is the ‘STOP 5’ debrief developed in Edinburgh by Dr Craig Walker’s team. A version used in Sydney is shown here:

References
1. I.R. Whitman, H.I. Feldman, R. Deo. CKD and sudden cardiac death: epidemiology, mechanisms, and therapeutic approaches. J Am Soc Nephrol, 23 (2012), pp. 1929-1939
2. Desbiens NA. Simplifying the diagnosis and management of pulseless electrical activity in adults: a qualitative review. Crit Care Med 2008;36(2):391-6
3. Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the Hospital: A Consensus Statement From the American Heart Association. Circulation. 2013 Jul 22;128(4):417–35
4. Rice DT, Nudell NG, Habrat DA, Smith JE, Ernest EV. CPR induced consciousness: It’s time for sedation protocols for this growing population. Resuscitation. 2016 Jun;103:e15–6
